Do Masks Really Work?

We have received a lot of questions from our patients and their families about masks over the past few months. To answer your questions, we’ve created this comprehensive resource guide about how masks work, what type of mask to wear, and when to wear them.
Wearing a mask in public settings remains a recommended practice to help prevent the spread of COVID-19 through community exposure. Exposure occurs when an infected person coughs, sneezes, or produces airborne contaminants in the environment. Reducing the risk of transmission is the key reasoning behind wearing a mask, and studies show that masks are an effective tool against the spread of COVID-19.
Wearing masks can help us from unknowingly spreading the virus to others and also help protect us from exposure. Continue reading to learn about how COVID-19 spreads, why you should wear a mask, the types of masks, how you can make your own mask, and how to properly wear a mask.
How Does COVID-19 Spread?
Current studies show that COVID-19 is primarily spread through respiratory droplets and aerosols. Droplets are “large particles of liquid usually produced by someone who has coughed or sneezed.” Droplets can spread onto high-touch surfaces where contamination can occur, including doors, desks, and countertops. Aerosols are much smaller in size and can remain in the air for extended periods of time. “In addition to being spread via coughs and sneezes, aerosols can also be released by talking or breathing.” Because there are a variety of ways the virus can spread through the air, wearing a mask can help protect you and the community from viral transmission.

Why Should I Wear A Mask?
 The biggest benefit of wearing a mask is to help prevent pre-symptomatic and asymptomatic COVID-19 carriers from spreading germs into the community. Masks provide an extra layer of protection against droplets traveling in the air and onto other people. While the effectiveness of masks may vary based on type, fit, and use, studies show that any barrier is better than none at all.
The biggest benefit of wearing a mask is to help prevent pre-symptomatic and asymptomatic COVID-19 carriers from spreading germs into the community. Masks provide an extra layer of protection against droplets traveling in the air and onto other people. While the effectiveness of masks may vary based on type, fit, and use, studies show that any barrier is better than none at all.
The CDC recommends wearing masks in public settings, especially when it is difficult to maintain social distancing guidelines (places like grocery stores, pharmacies, religious services, gyms, and other high density, enclosed spaces). Remember, masks are not a substitute for Social Distancing guidelines. Continue to observe both, especially in areas at high risk for community-based transmission.
What About Double Masking?
 Properly wearing a single mask has been shown to be effective in reducing the risk in getting and spreading COVID-19. “We continue to recommend that masks should have two or more layers, completely cover your nose and mouth, and fit snugly against your nose and the sides of your face,” said CDC Director Dr. Rochelle Walensky (via CNN). Other than ensuring proper mask usage, new studies indicate there may be added value to double masking. The CDC has released updated guidelines on improving mask protection, recommending wearing a disposable mask closest to the face, followed by a layered cloth mask. Double masking can provide extra protection in high traffic environments, such as public transportation, trains, and airports.
Properly wearing a single mask has been shown to be effective in reducing the risk in getting and spreading COVID-19. “We continue to recommend that masks should have two or more layers, completely cover your nose and mouth, and fit snugly against your nose and the sides of your face,” said CDC Director Dr. Rochelle Walensky (via CNN). Other than ensuring proper mask usage, new studies indicate there may be added value to double masking. The CDC has released updated guidelines on improving mask protection, recommending wearing a disposable mask closest to the face, followed by a layered cloth mask. Double masking can provide extra protection in high traffic environments, such as public transportation, trains, and airports.
What If I’m Healthy?
One of the critical concerns with the spread of COVID-19 is that those who are infected may not show symptoms or even know that they are sick. A variety of recent studies show anywhere from 25% to 80% of people with COVID-19 are unaware they have the virus. Those that are infected can inadvertently transmit the virus days before showing symptoms, with an estimated 44% of transmissions occurring between people before the carrier started showing symptoms.
 While testing has been developed and distributed in an effort to diagnose those with COVID-19 and identify antibodies, there are concerns regarding accuracy. Many tests require blood testing to be validated with a nasal swab, and may not necessarily be accurate indicators of exposure. Due to both false positives and false negatives, it may be necessary to repeat nasal testing for those who express symptoms consistent with COVID-19.
While testing has been developed and distributed in an effort to diagnose those with COVID-19 and identify antibodies, there are concerns regarding accuracy. Many tests require blood testing to be validated with a nasal swab, and may not necessarily be accurate indicators of exposure. Due to both false positives and false negatives, it may be necessary to repeat nasal testing for those who express symptoms consistent with COVID-19.
AdventHealth recently reported significant concerns about COVID-19 testing, stating that more than 25,000 tests performed in Central Florida may be unreliable.
Studies and testing are ongoing and continue to teach us more about the virus, but it is difficult to know who is infected. Wearing a mask is the safest way to help protect others and ourselves from community exposure. Consider the adage, “My mask protects you, your mask protects me.”
What Types of Masks Are There?
The main types of masks are N95 Respirator Masks, Surgical Masks, and Cloth Masks.
N95 Respirator Masks

N95 Respirators are masks that should remain reserved for health care workers. N95 masks are fit tightly on the face in order to create a seal, which helps filter about 95% of particles. Because these masks are in short supply, it is critical that they are worn by healthcare professionals who are evaluating and performing procedures on patients diagnosed with COVID-19. According to the CDC, “the cloth face coverings recommended are not surgical masks or N-95 respirators. Those are critical supplies that must continue to be reserved for healthcare workers and other medical first responders, as recommended by current CDC guidance.”
Note: Masks with filters that allow air to be released from the mask defeat the purpose of preventing the spread of potential contagions into the environment.
Surgical Masks

Surgical masks are the most common masks worn by healthcare workers and are effective against large droplets. These masks do not require sizing and are a loose-fitting, unlike N95 masks. While these masks are still recommended primarily for healthcare workers, surgical masks are a viable options for those who are unable to make their own. Surgical masks are meant to be discarded after they are worn and should not be reused. Repetitive use of these masks can lead to self-contamination.
Note: Do not attempt to sanitize disposable/surgical masks. Leaving a used mask in the car or heat does not guarantee the mask has been sanitized. Placing a mask over steaming water does not guarantee the mask has been sanitized. Masks may be reused if adhering to strict 5-day alternating window between wearing.
Cloth Masks
 Cloth masks can be made using a variety of fabrics, including t-shirts, bandanas, scarves, and more. It’s important to ensure they properly cover your nose and mouth. Cloth masks should only be used one time within the day and should always be cleaned after being worn. Never touch the outside of your mask for positioning. If you must touch your mask, be sure to wash your hands afterwards so you do not spread any potential contaminants from the outside of the mask.
Cloth masks can be made using a variety of fabrics, including t-shirts, bandanas, scarves, and more. It’s important to ensure they properly cover your nose and mouth. Cloth masks should only be used one time within the day and should always be cleaned after being worn. Never touch the outside of your mask for positioning. If you must touch your mask, be sure to wash your hands afterwards so you do not spread any potential contaminants from the outside of the mask.
While the effectiveness of cloth masks may vary based on their material, studies show they are far better than no mask at all and effectively block most large droplets as well as some fine droplets. Research regarding the most effective fabrics and layers to filter out infectious particles is visualized below in this graphic by the University of Nebraska Medical Center. The better the mask material is, the more effective it is at filtering droplets.
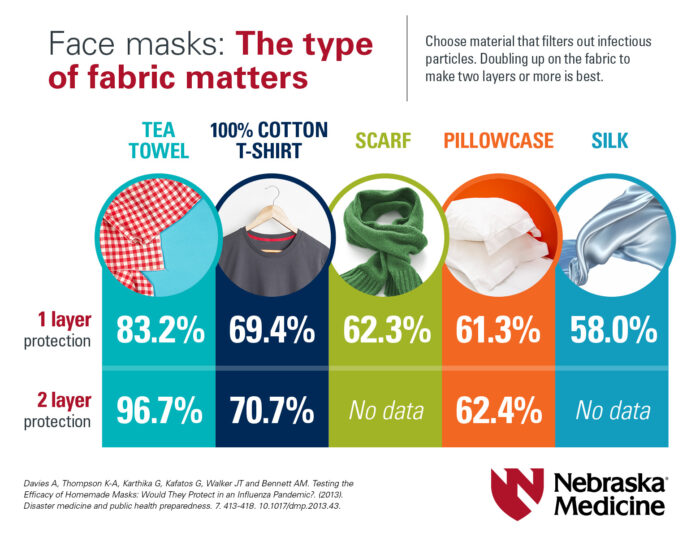
Note: Recent studies on effectiveness of mask materials show that items like bandanas and fleece coverings are not as effective as cotton and other materials.
How Do I Wear A Mask?
When wearing a mask, make sure to follow the CDC guidelines to ensure you are wearing it correctly. Cloth masks should be worn for no more than four hours at a time before being washed in hot water and thoroughly dried. Avoid touching the mask and wash your hands immediately if you do. Wear your mask correctly by making sure that:

- The mouth and nose are fully covered. The mask should reach above the bridge of your nose and below the chin. Fit is important. A mask should be snug.
- The covering fits snugly against the sides of the face so there are no gaps.
- You do not have any difficulty breathing while wearing the mask.
- The mask can be tied or secured to prevent slipping.
- If using a cloth mask, wash after each use in the washing machine or by hand using a bleach solution and allow it to dry completely.
Note: The area around and over the nose presents the highest opportunity for leakage. Be sure that the mask fits snugly around your nose and face in order for it to be as effective as possible.
How Do I Put On and Take Off My Mask Safely?
Putting on and taking off your mask properly is extremely important in order to prevent self-contamination. Make sure to:

- Wash your hands before you handle your mask, when putting it on and when taking it off.
- Handle the mask with care, using only the ear loops or ties to put it on and take it off.
- Make sure the mask properly covers both your nose and mouth.
- Gently pat the mask around your face to seal it around your nose and chin.
- Be sure to wash your hands any time you touch your mask to avoid self-contamination.
- Do not leave the mask lying around after use, be sure to either dispose of it or wash it in order to prevent germs from spreading.
Watch this quick video on the proper procedure for handling masks by the University of Nebraska Medical Center.
What If I’m Having Trouble Breathing With A Mask?
Certain mask materials can restrict airflow and make it more difficult for people to breathe, especially those suffering from asthma, allergies, COPD, and other respiratory diseases.
If you are having trouble breathing while wearing a mask, consider the following:
 Make sure you use the right mask. N95 masks are not recommended for heavy activity use or for those who are not directly involved in healthcare.
Make sure you use the right mask. N95 masks are not recommended for heavy activity use or for those who are not directly involved in healthcare.- Surgical masks are loose-fitting and should allow for more airflow.
- Reduce going out to limit mask wearing.
- Cotton-based masks may cause feelings of asphyxiation for those with breathing issues.
- Paper towel masks (2-ply) or shop towel masks may provide more airflow when breathing.
- Neck gaiters, fleece, and bandanas are less viable alternatives to other materials and do not provide the same amount of protection.
What If I Have Additional Concerns?
Send us a message in Patient Portal or Book An Appointment to talk to your Clinical Team more in-depth about your concerns with COVID-19 and your risk factors. For further information on COVID-19, please visit our Patient Advisory page.
—
Disclaimer: All information presented on this website is intended for educational purposes only and not intended to replace your individual medical advice. Please review this information with your clinical team to ensure it is appropriate for your individual medical needs. The information contained is not intended to diagnose, treat, cure or prevent any disease.
